
Prostatitis in men is an inflammatory process involving the prostate tissue. This disease is accompanied by pain that occurs in the lower back, perineum, and pelvis. The main manifestations are perineal pain and lower urinary tract dysfunction.
Of all the urological disorders, prostatitis is the most commonly encountered by urologists. It can develop suddenly (acutely) in the context of general health, or persist for a long time, with periods of exacerbations and remissions, suggesting a chronic course. In addition, a second variant of the disease was diagnosed more frequently.
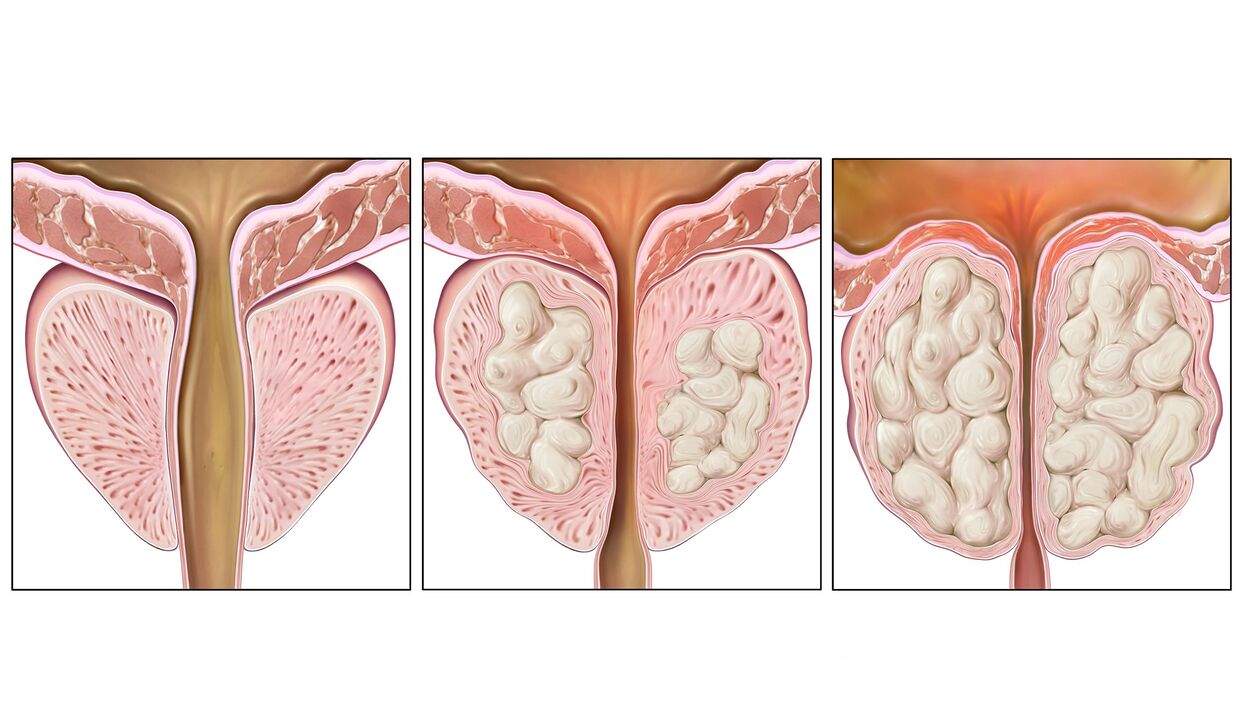
The disease exists independently, and can also be combined with benign prostatic hyperplasia or prostate cancer.
Development reasons
Inflammation does not appear alone. The etiology of prostatitis can be divided into bacterial and non-bacterial.
Acute infectious variants usually occur in men under the age of 35 due to damage to the prostate by Gram-negative bacteria (Escherichia coli, Proteus, Enterobacter). In addition, inflammation occurs due to infection with sexually transmitted infections - gonorrhea, chlamydia. In the chronic form, there may be more causes, and the list will include atypical organisms.
Predisposing factors for the development of bacterial variants are:
- unprotected sex;
- AIDS or HIV infection;
- diarrhea or constipation;
- anal sexual contact;
- a sedentary lifestyle;
- sexual inactivity;
- diabetes;
- low temperature;
- Violation of privacy hygiene.
- mood disorders;
- autoimmune diseases;
- increase physical activity;
- Lack of regular sex life;
- work related to weightlifting;
- chronic stress;
- Congestion of prostate tissue;
- Previously demonstrated fibrotic changes in the prostate (according to TRUS results).
What are the first signs of prostatitis?
The initial manifestations of the disease are pain in the waist and perineum, and difficulty urinating. If you notice a diminished urine flow, discomfort, or burning sensation in your urethra when using the toilet, you should contact your urologist as soon as possible.
With an acute onset of illness, temperatures may rise and overall health may deteriorate. Such patients should be treated immediately by connecting antibiotics, anti-inflammatory drugs.
In some cases, the disease can be asymptomatic for a long time, so treatment starts late.
Symptoms of prostatitis
Symptoms of prostatitis in men depend on the form of the disease. In the acute form, the following manifestations are characterized:
- Pain in the lower back, sacrum, perineum;
- frequent or difficult urination;
- acute urinary retention;
- Difficulty defecating;
- a thin stream of urine;
- temperature rise;
- chills;
- General well-being worsens.
The chronic form may occur after the acute phase of the disease or develop into a primary disease. Prostatitis symptoms are milder in men with a chronic course. Pain intensity is low and body temperature may be slightly elevated. The urine stream becomes thinner, and disturbances appear in the intimate realm.
During the chronic course, exacerbation of prostatitis with symptoms characteristic of the acute phase may occur. Pain may be absent or have a dull aching character.
Symptoms of acute prostatitis
Acute prostatitis occurs in several stages, which can pass from one to another if you do not contact a specialist and stop the development of the disease in time.
The first stage is called acute catarrhal prostatitis. It starts with complaints of frequent painful urination. In the lower back and sacrum and perineum, there will be mild soreness at first, and then it will increase rapidly.
If left untreated, a second stage occurs - acute follicles. At this time, the pain is particularly severe, radiating to the anus, and aggravated during defecation. Urination is very difficult and sometimes acute urinary retention occurs. The temperature does not exceed 38 degrees, and only in rare cases higher.
Acute substantive prostatitis manifests as severe poisoning, body temperature above 38°C, and chills. Urinary retention, sharp throbbing pain in the perineum, and difficulty with defecation are often observed.
Symptoms of Chronic Prostatitis
Sometimes chronic prostatitis occurs against the background of an acute inflammatory process. It is an independent disease in which there is a primary chronic course that develops over a long period of time.
As a rule, the chronic course begins with complications of the inflammatory process caused by various infectious agents - chlamydia, trichomonas, gonorrhea. But there are few vivid manifestations, mostly urination or slight pain in the perineum, and a small amount of discharge from the urethra. Often, these manifestations are not even noticed by the patient for a long time.
Symptoms of prostatitis in men can appear in different ways, but they can all be grouped into three categories - pain syndrome, urinary disturbances, sexual problems. Prostate tissue has no receptors, so they cannot produce pain. They appear when inflammation begins to migrate to the innervated rich pelvic organs. Patients' pain can vary - from barely noticeable discomfort to intense and excruciating discomfort, which disrupts sleep and habitual lifestyle. Pain can radiate to the sacrum, scrotum, lower back, and perineum, and self-diagnosis is useless here.
Urination problems begin the moment the prostate increases in size and begins to squeeze the urethra, reducing the lumen of the ureters. Frequent urination, feeling of not being able to empty the bladder. Usually, such phenomena appear at the very beginning, early stages of the disease, which are then compensated by the body, but at a later stage, without proper treatment, they reappear.
Potency issues in men can also be expressed in different ways. Patients complain of worsened erections, accelerated ejaculation, and decreased sexual arousal. Gradually, sexual dysfunction becomes more obvious, and in the advanced stage, the symptoms of prostatitis are accompanied by impotence.
Classification
Experts divide diseases into several categories:
- Acute bacterial prostatitis, characterized by symptoms of bacterial infection. In most cases, the causative agent of the disease is Escherichia coli. In less cases, enterococci and other bacteria were isolated;
- Chronic bacterial prostatitis, which is a recurring disease. The pathogens of the disease are Escherichia coli, Enterococcus and the like. Trichomonas, fungi, chlamydia, viruses, and mycoplasma can also become pathogens;
- Chronic pelvic pain syndrome in which no infection is detected. There are two types: inflammatory and non-inflammatory. Causes include: autoimmune processes, external factors (hypothermia, overheating), infrequent sex life, low physical activity, infrequent urination;
- Asymptomatic prostatitis discovered incidentally during physical examination.
Only qualified specialists can accurately name the type of prostatitis according to the examination data, and determine the treatment plan after a thorough diagnosis. If you have certain signs, you should contact a specialist.
symptom
The main symptom is a violation of the functions of the urinary system. You should contact a specialist if you have:
- If you have difficulty urinating and passing urine intermittently;
- If there is discharge from the urethra during a bowel movement;
- Burning sensation in the urethra and perineum;
- If you have bladder and prostate discomfort during bowel movements;
- if the urge to urinate increases and becomes more frequent;
- if you have rectal pain;
- If the urethra has a purulent bloody discharge (floating "threads");
- Frequently elevated body temperature;
- With the onset of intimacy problems (weakened erections);
- when erections occur at night for unexplained reasons;
- If you ejaculate too quickly during intercourse;
- If the sensation during orgasm is "erased";
- rapid general fatigue;
- exhibits an unreasonable state of anxiety or depression, as well as a depressed state of mind;
- Frequently depressed, showing mental depression in anticipation of complications;
- General weakness.
In order to contact a urologist, one or two symptoms are enough. Often, attempts to heal on their own lead to exacerbations, with the disease turning into a chronic or severe form. In worst-case scenarios, failure to seek immediate medical attention can result in infertility or outright impotence.

If the patient does not seek medical attention in time or neglects treatment, the following symptoms may occur:
- Perineal pain;
- pain near the scrotum;
- Pain (pain) at the base of the penis.
Pain indicates stone formation. Doctors refer to infertility as a late sign of a progressive disease.
Symptoms of acute and chronic forms of prostatitis differ significantly. In particular, in the chronic form, signs may be mild or not manifest at all.
Acute prostatitis is characterized by pronounced symptoms - general malaise, pain in the groin area. Men need to contact a specialist if:
- The urge to urinate becomes very frequent;
- Pain that worsens in the perineum and radiates to the groin during defecation and urination;
- It is impossible to completely empty the bladder;
- A marked decrease in the amount of urine formed or not collected each day;
- Fever, frequent headaches, general weakness.
Acute bacterial prostatitis is characterized by fever, chills, lumbosacral pain (strong), perineal and rectal pain, acute urinary retention, and often painful muscles and joints.
Chronic prostatitis has the following symptoms:
- Increased pain in the perineum when urinating;
- frequent urges, bladder not fully emptied;
- decreased libido;
- Discomfort during sex.
One of the hallmarks of the chronic form is a marked disturbance of the emotional background, characterized by insomnia, increased nervousness, capriciousness, irritability.
The bacterial form of chronic prostatitis is characterized by problems with ejaculation that becomes quick and painful, genital discomfort, frequent or involuntary urination, and intermittent urine stream.
Chronic pelvic pain syndrome, according to medical statistics, is the most common form of prostatitis with symptoms similar to those of chronic bacterial prostatitis: frequent urination, decreased urine flow, pain in the penis, pain in the testicles, sexual dysfunction.
possible complications
- Vesiculitis;
- Posterior urethritis or conjunctivitis;
- abscess of the gland itself;
- hardening or fibrosis of the prostate gland;
- prostate cysts and stones;
- infertility;
- ejaculation disorders;
- Erectile dysfunction.
diagnosis
Urologists diagnose and treat any form of prostatitis. If a tumor is suspected, the patient may be referred to an oncologist for consultation. For chronic, long-standing prostatitis that is difficult to treat, consultation with an immunologist may be necessary.
- Urine bacteriological culture.
- Microbiota and susceptibility to antibiotics analyzed in prostatic secretions.
- Prostate rectal examination.
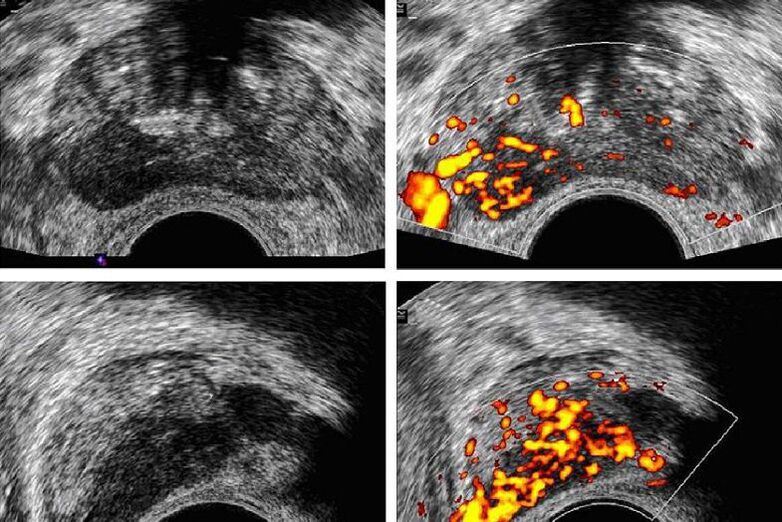
- Ultrasound of the prostate can identify tumors, cysts, adenomas, and differentiate prostatitis from other urological and surgical disorders.
- Sperm pattern ruled out infertility.
Diagnostic features of acute prostatitis
If the signs of the disease indicate acute prostatitis, the diagnosis is made on the basis of instrumental and clinical examination data. Any procedures that could affect the prostate are contraindicated because they can cause severe pain or allow the infection to spread.
Diagnostic Features of Chronic Bacterial Prostatitis
The diagnosis in this case is determined on the basis of the following data: examination of the patient's doctor, bacteriological and microscopic examination of prostatic secretions, study of ultrasound data.
Diagnostic features of pelvic pain syndrome
Taking into account the type of disease: inflammatory or non-inflammatory, the specialist develops a diagnostic procedure for symptoms indicative of chronic pelvic pain syndrome. As a rule, ultrasound prescribes, as well as the following procedure:
- Prostate secretion research;
- molecular biology research;
- Bacteriological research.
The choice of technique is determined by the doctor based on the initial examination.
high risk group
Prostatitis is most likely to occur and develop in:
- In obese or sedentary men;
- Sedentary men (office workers, programmers);
- Men whose bodies are shaken and vibrated (car drivers, including special equipment);
- Men with infectious diseases, including diseases of the genitourinary system;
- In sexually hyperactive men and men who are sexually infrequent;
- Depressed, mentally ill men;
- In alcoholics, drug addicts, etc.
treat
Patients with confirmed acute prostatitis but no complications were treated on an outpatient basis. Hospitalization is carried out only in the presence of severe symptoms of intoxication and suspicion of a purulent process.
Antibiotics are the drug of choice to fight inflammation. They are also used in chronic bacterial form. Drugs are selected individually and taken as a course of 4-6 weeks. In severe cases, the antiseptic is administered intravenously, in all other cases - orally in the form of capsules or tablets.
Another drug used for prostatitis is an alpha1 receptor blocker, which is prescribed in the presence of residual urine confirmed by ultrasound. They help promote urination and relax the muscles of the prostate and bladder. NSAIDs can help relieve pain.
Treatment of prostatitis can only be done comprehensively and consistently. In addition to medication, your doctor will prescribe a course of prostate massage and use physical therapy to improve circulation to this organ. Surgical treatment is used only in cases of seminal vesicle abscess and suppuration.

The choice of prostatitis treatment depends on many factors and is determined individually. When choosing a treatment approach, the following factors should be considered:
- the cause of the disease;
- course of disease;
- Individual characteristics of the body (presence of chronic and concomitant diseases).
For treatment, a specific technique may be chosen or a complex may be prescribed. Based on the results of the diagnosis, specialists in the field of urology prescribe:
- Physiotherapy procedures: magnetic resonance therapy, procedures using laser equipment, ultrasound, reflexology, massage, leech therapy.
- medical treatement.
- Diet and psychotherapy.
- operation treatment.
When diagnosing bacterial prostatitis, broad-spectrum antibiotics, immunomodulators, and multivitamin complexes are prescribed.
Physiotherapy and anti-inflammatory drugs are prescribed when nonbacterial prostatitis is diagnosed.
In some cases, specialists may recommend muscle relaxants and hormone therapy, along with antioxidants that help reduce inflammation and protect cells from free radicals.
Properly selected drug complexes for acute bacterial prostatitis:
- restore immunity;
- treatment of infection (antibiotics);
- Treatment of the prostate (antibacterial medicine).
Chronic prostatitis is difficult to treat, so an extensive list of drugs is used: anti-inflammatory drugs, antispasmodics, absorbable drugs, antibacterial drugs, vibration massage and finger massage, electrophoresis, EHF and UHF therapy, sinusoidally modulated currents.
When diagnosing pelvic pain syndrome, antibiotics and anti-inflammatory drugs, various physical therapies, magnetic therapy and laser therapy, electrical nerve stimulation, etc. , one of the effective methods is tissue drainage around the inflammatory lesion.
Urologists choose conservative or modern treatment based on diagnostic data.
tablet
Antibacterial agents, pain relievers in the form of tablets can be prescribed for prostatitis.
The course of antibiotic therapy is selected individually on the basis of the results of the analysis of the prostatic secretions. Disease-causing microbial communities must be sensitive to the drugs used. The course of treatment prescribed by the urologist must be completed, otherwise the cause will not be eliminated and the disease will recur or become chronic.
Prostatitis pain relievers can help eliminate unpleasant symptoms. For this, use NSAIDs, which not only eliminate pain but also relieve inflammation.
Prostatitis drugs for men that help with voiding disorders are alpha1-blockers. They relax smooth muscle and restore patency to the urethra, which is squeezed by the inflamed prostate.
prostatitis injection
Antibacterial agents for prostatitis in men are also available in the form of injections. The injectable form of the drug is used to treat severe inflammation, and in the absence of antibiotics in tablet form, to which pathogens are susceptible. You can inject antispasmodics to quickly resume urination, which can be difficult due to spasms in the urinary tract and pressure on the prostate.
Injectable prostatitis medications work faster than oral medications and are therefore sometimes preferred.
Prostatitis Surgery
The most dire complications are seminal vesicle suppuration and abscesses. In such a difficult case, the medicines used to treat the disease do not cope with the disease, therefore, surgery is required at the first manifestations.
In the absence of timely intervention, the purulent process can spread beyond the organ, so the consequences of complex forms of prostatitis can be life-threatening.
Prediction and Prevention
The untreated acute form often becomes chronic, with periodic exacerbations. A full recovery is not always possible, but seeing a doctor promptly and taking all prescribed medications can eliminate discomfort, urination problems, and pain.
Self-treatment at home and using folk methods are often life-threatening.
To prevent prostatitis, it is recommended to avoid hypothermia, empty the bladder promptly, limit the use of coffee, spices, and alcohol, and remain sexually active for as long as possible.
Typical Symptoms of Prostate Cancer
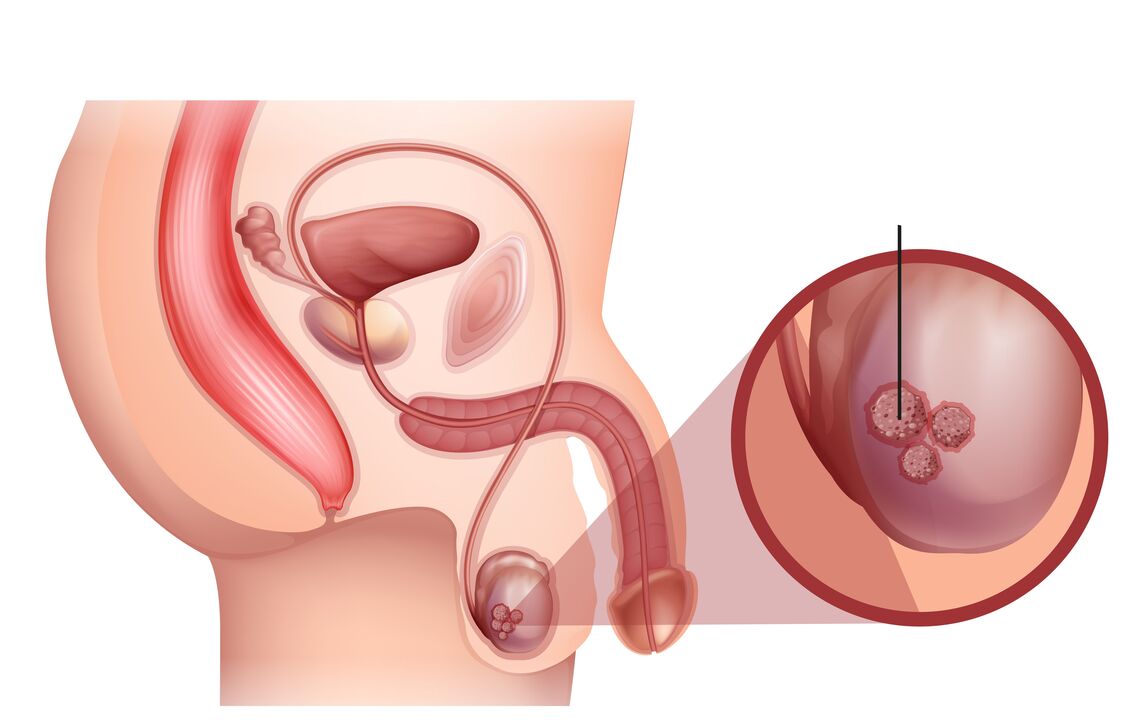
The prostate is a small organ found only in men. It has a sponge-like structure that sits below the bladder and wraps around the urethra. Under the influence of male hormones, the gland begins to grow during puberty; by adulthood, it can weigh up to 20 grams. It plays an important role in the male reproductive system, produces a secret, and is one of the components of sperm. But unfortunately, in mature and elderly men, glandular hyperplasia or malignant tumors of organs are often found.
How to recognize cancer
As the tumor grows and progresses, symptoms of prostate cancer depend on the stage of the process. If the disease is still in stage 1 or even reached stage 2, the tumor is located within the prostate, has not grown into adjacent tissue and is not allowed to metastasize.
There are almost no early symptoms of prostate cancer, which is the hidden nature of the disease. The man had no complaints, felt fine and saw no reason to see a doctor. This is why this type of tumor is often found in an already neglected state. An exception may be patients who have previously been diagnosed with a benign tumor of the prostate, in which case they are regularly observed by a specialist and tested for specific prostate antigen and ultrasound of the gland. They have a chance to detect it at the onset of the tumor. But it's worth noting that detecting prostate cancer isn't always easy. Even with a biopsy, the results may be clear, but the oncology has it. This is due to an error in the method, where the needle does not fall into the local focus at all. If something is suspected about the prostate, especially cancer, a fusion biopsy should be done, which combines the capabilities of ultrasound and MRI in real time, giving doctors the opportunity to see the organ as accurately as possible.
Some symptoms are the result of prostate pathology, while others are caused by mechanical compression and obstruction of the urethra.
Since the bladder must be emptied on a regular basis, if this process is disturbed, urine can become lodged in it, inflammation can occur, and a bacterial infection can develop. If nothing is done, the process will spread, which already threatens pyelonephritis and kidney problems.
In stage 4, the manifestations of prostate cancer are more pronounced. Metastasis most commonly occurs in the bones, spine, and lymph. As a result, a person's regional lymph nodes can grow, bones can hurt, and they can lose weight dramatically and become weak.
Treating prostate cancer is not easy, but it can be done. By detecting local processes in time, complete healing can be achieved and, in more advanced stages, lifespan can be prolonged. If you find the above symptoms, please contact a professional clinic for examination.
Make an appointment, the clinic's doctors have many years of experience in the treatment of urological diseases and are able to succeed even in the most difficult cases.






























